Shout out to Dr. Akkad for her excellent case last week on a 51 year old woman with history of HTN, obesity and hyperlipidema who presented with progressive shortness of breath, fatigue and altered mental status for 1 week.
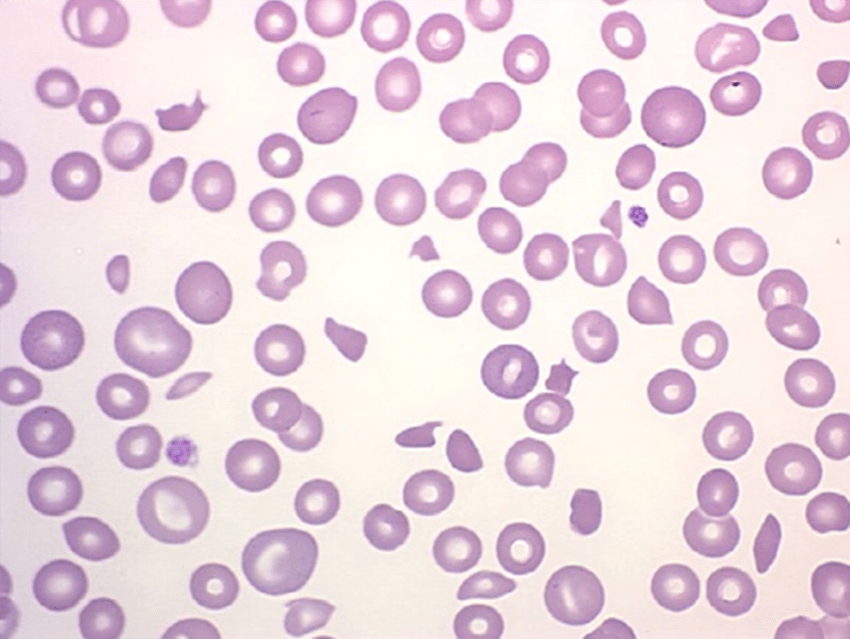
Work up revealed that the patient was anemic and thrombocytopenic. Peripheral smear showed schistocytes (see above) and the patient had an ADAMSTS13 <5%, sealing the diagnosis of Thrombotic Thrombocytopenic Purpura (TTP).
Key takeaway points from the case:
- Always have a high index of suspicion as this is a life-threatening disease requiring emergent therapy once identified.
- Look at the Smear!!!!
- The PLASMIC Score can be calculated for patients who you may suspect have TTP to help determine their risk (low/intermediate/high) of having TTP (View link)
- The level of renal dysfunction is not as severe as would be seen in other TMAs (ex. Atypical HUS, drug induced etc.) and oftentimes the Cr <2.0
- Treatment: PLEX or caplacizumab
One of our wonderful new General Medicine fellows, Kevin Stephenson, provided us some interesting tidbits about TTP:
- Stroke and TTP: TTP presenting as stroke appears to be uncommon in younger (<60yo) patients. I found a handful of case reports, and I believe all of them described patients with known TTP presenting with relapse as stroke. In these patients with known TTP, the combination of thrombocytopenia and stroke prompted PLEX. Fascinatingly, their neuro syndromes all improved with PLEX
- Is Haptoglobin always undetectable? Haptoglobin is extremely sensitive in some causes of hemolysis, particularly AIHA, but less sensitive in TMAs specifically. The main hypothesis given is that haptoglobin is also an acute phase reactant, so when there is inflammation as well as hemolysis, the balance is tipped enough toward production of haptoglobin (5-6 day half life) to give a “low-normal or normal range” value despite ongoing destruction (half life of haptoglobin-hemoglobin complex 15 minutes). Interesting corollary I would posit – if the patient is inflamed (sometimes the case in TTP, often in infection-related TMAs) and has a low-normal haptoglobin, we should perhaps be more suspicious for hemolytic anemia than we might otherwise be, because it really should be increased in these patients (except with cirrhosis and a few other caveats).
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4706896/
- https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.23249
Thanks Neha and Kevin!